
In a world dominated by screens and constantly changing visual stimuli, maintaining our eyesight has never been more important. According to the Center for disease control (CDC), a whopping 12 million Americans aged 40 and over suffer from varied degrees of vision impairment. However, the damage extends beyond age, affecting our youngest generation, with nearly 7% of children suffering from identified eye and visual issues.
As we delve into ocular health, this article aims to shed light on six (6) common eye diseases that affect individuals across the age spectrum. Beyond mere identification, we explore both traditional clinical interventions and emerging holistic approaches, with focus on the innovative Anywhere Healing Alpha Heal Device, striving to redefine how we perceive and protect our precious gift of sight.
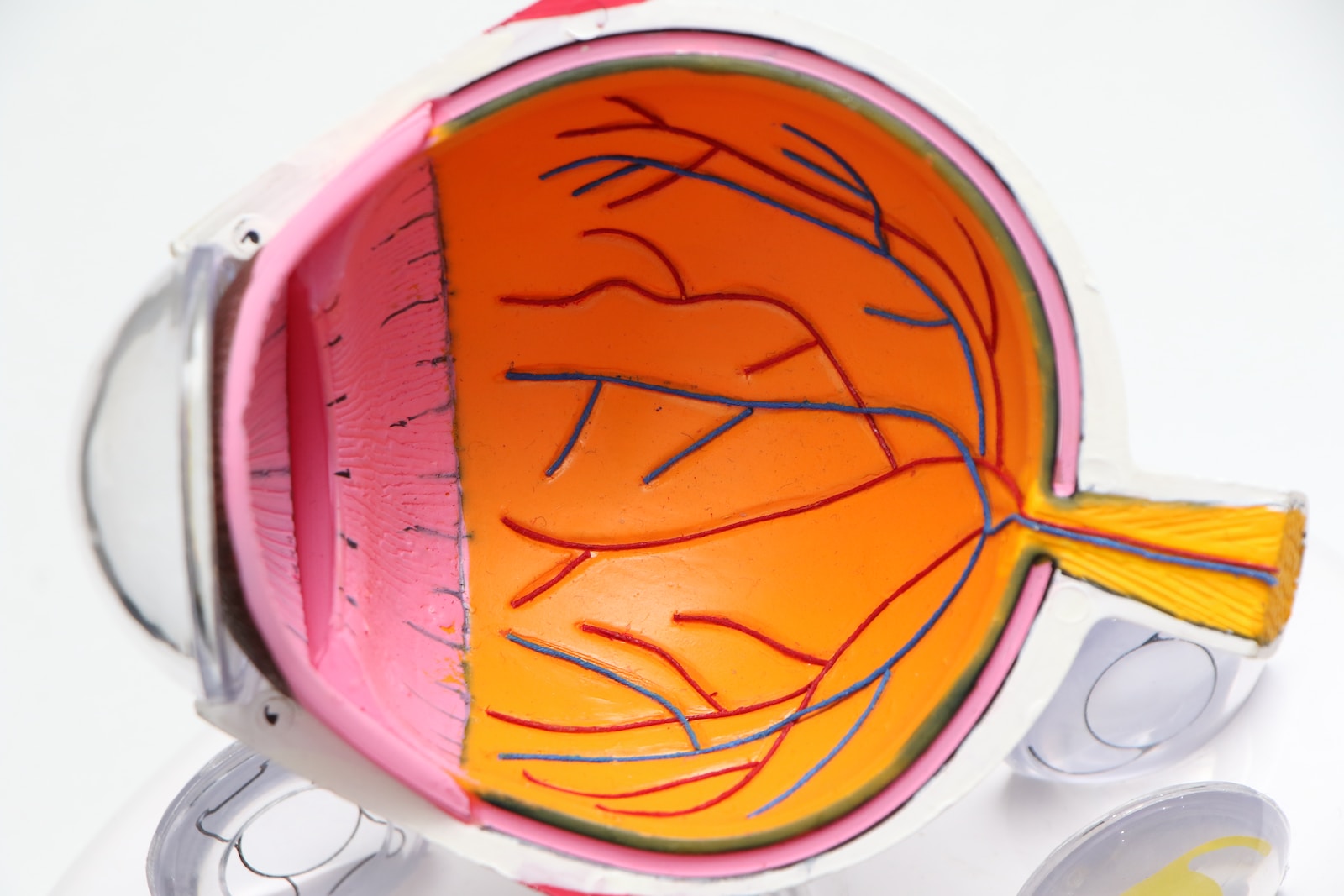
Refractive errors are common enemies of visual acuity. Myopia, also known as nearsightedness, occurs when distant things look blurry as a result of light focusing in front of the retina. As light converges behind the retina, hyperopia, or farsightedness, causes difficulty with close-up work. Astigmatism, a complex cornea curvature, affects both near and far vision. The optical subtleties that govern how light traverses and converges within the eye cause this trifecta of refractive aberrations.
Myopia manifests itself as squinting or difficulties recognizing distant faces, whereas hyperopia can cause eye strain and headaches when performing close tasks. Astigmatism causes visual abnormalities as well as discomfort. These errors, when added together, have a widespread impact on daily tasks, affecting everything from reading a book to traversing the outlines of a faraway terrain.
Precision comes in the form of corrective lenses and novel surgical treatments to control refractive problems. Corrective lenses, whether glasses or contact lenses, function as optical aids, refracting light so that it aligns with the retina. LASIK surgery, a more advanced procedure, reshapes the cornea to cure refractive errors. This surgical procedure provides a freeing alternative for those desiring less reliance on external visual assistance, changing the vision correction landscape.
Beyond the clinical hallways, holistic methods of refractive error management carve a niche. Eye exercises, a practice designed to strengthen ocular muscles and increase concentrating ability, are a non-invasive way to improve vision. Nutritional considerations, with a focus on vitamins A, C, and E, as well as minerals such as zinc, nourish ocular tissues and support general eye health. The combination of eye exercises and a nutrient-rich diet highlights the possibility of improving visual well-being holistically.

Macular degeneration manifests in two separate forms—dry and wet—in the delicate nuances of retinal physiology. The dry form manifests itself over time as a gradual breakdown of light-sensitive cells in the macula, resulting in a slow but progressive loss of central vision. On the contrary, the wet version, while less common, has a more aggressive disposition. Abnormal blood vessel growth behind the retina, combined with possible fluid and blood leakage, hastens the deterioration of central vision.
Navigating the clinical landscape of macular degeneration necessitates a keen understanding of its risk factors and early symptoms. Age, an indisputable protagonist, asserts its influence, with advanced years correlating to an increased vulnerability. Genetic predisposition, smoking, and a dearth of protective nutrients further elevate the risk. Early symptoms may present as distorted or blurry vision, a precursor to the insidious progression of central vision impairment.
Clinical therapies serve as foundations of fortification in the fight against macular degeneration. Anti-VEGF therapy, a novel technique, works by preventing the formation of aberrant blood vessels behind the retina. The therapy halts the progression of the aggressive wet type by reducing the danger of leakage and bleeding. At the same time, laser therapy plays a strategic function, attempting to seal leaking blood vessels while also strengthening the structural integrity of the macula.
Antioxidant-rich dietary supplements, such as vitamins C and E, zinc, and copper, provide a protective shield against oxidative stress, lowering the risk of degeneration. Aside from the pillbox, lifestyle adjustments demand consideration. Smoking reduction, along with a diet rich in leafy greens, fish, and nuts, is a comprehensive approach to improving macular resilience.
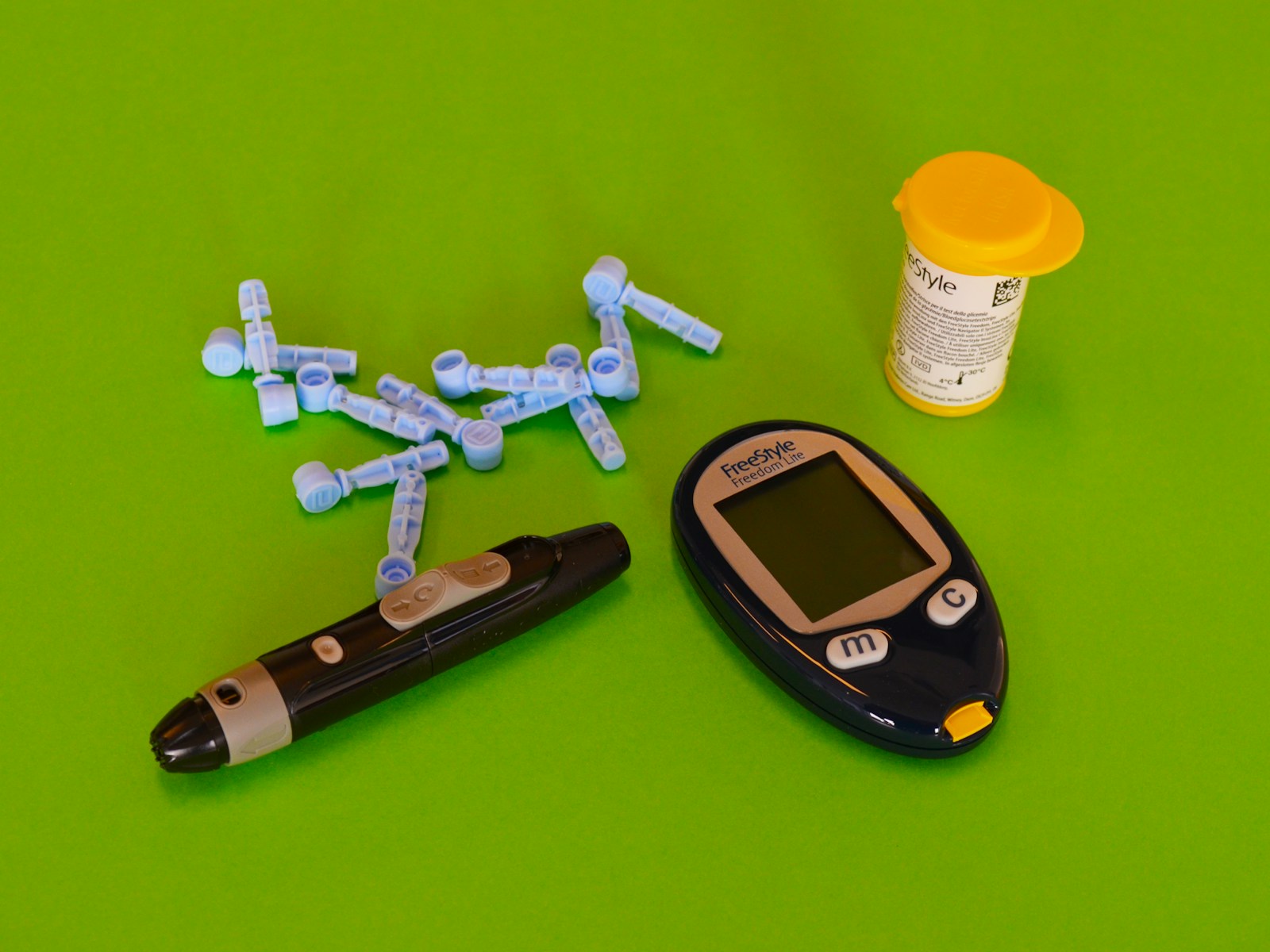
It is imperative to recognize its intrinsic link between Diabetic retinopathy and diabetes mellitus. This ocular complication arises as a consequence of prolonged exposure to elevated blood sugar levels, a hallmark of diabetes. Given the escalating global prevalence of diabetes, diabetic retinopathy has become a formidable concern, emerging as a leading cause of vision impairment and blindness among the diabetic population.
The landscape of diabetic retinopathy unfolds across stages, each characterized by distinct ocular manifestations. In the early stages, microaneurysms and small hemorrhages manifest, often unnoticed by the individual. Progression leads to the development of more severe symptoms, including macular edema and proliferative changes marked by abnormal blood vessel growth. Symptoms range from subtle blurring of vision to pronounced visual distortions, demanding vigilant clinical scrutiny to curtail further progression.
Laser surgery, specifically focal and panretinal photocoagulation seal leaking blood vessels and abate abnormal vessel growth. Intraocular injections, often containing anti-VEGF medications or corticosteroids, further attenuate the inflammatory processes and angiogenesis. These interventions aim not only to salvage existing vision but also to forestall the relentless advancement of diabetic retinopathy.
Holistic treatments are crucial in the treatment of diabetic retinopathy. The most important of these is strict blood sugar control, which is essential in preventing and minimizing diabetes's ocular consequences. Regular eye exams, performed consistently, provide a proactive approach to early detection. These evaluations serve as an important conduit for timely intervention, allowing therapeutic techniques to be implemented before irreversible damage occurs.

The delicate dance of intraocular pressure (IOP) is at the heart of glaucoma, a disorder that threatens visual clarity. Elevated IOP becomes a prominent character in the story, exerting unnecessary pressure on the optic nerve. If left unchecked, this pressure causes a chain reaction of events that can result in irreversible eyesight loss. Understanding the delicate balance of IOP is critical in uncovering the mystery of glaucoma.
Glaucoma manifests itself clinically in a variety of ways, with primary open-angle glaucoma and angle-closure glaucoma taking center stage. Primary open-angle glaucoma is a sneaky foe that develops gradually and frequently without warning. Angle-closure glaucoma, on the other hand, is characterized by rapid and dramatic symptoms such as significant eye pain, headache, impaired vision, and halos around lights. Recognizing these indications is critical for rapid diagnosis and management of this eye disease.
The cornerstone of pharmacological intervention is topical eye drops, which aim to either reduce aqueous humor production or improve drainage. Surgical procedures ranging from trabeculectomy to laser trabeculoplasty are designed to reduce intraocular pressure by increasing fluid outflow. To optimize outcomes, the intervention of choice is dependent on rigorous evaluation and tailored treatment regimens.
Yoga reduces stress and improves overall well-being by emphasizing controlled breathing and gentle physical postures. Stress, which is frequently an aggravating factor, can have a major impact on IOP. As a result, stress management strategies such as mindfulness, meditation, and relaxation exercises play an important part in the overall armamentarium against glaucoma. These solutions provide a synergistic approach to traditional treatments by treating the psychosomatic components.
Amblyopia, colloquially known as Lazy Eye, and Strabismus stand as distinctive entities. Amblyopia manifests when the visual cortex inadequately develops due to unequal visual input from the eyes, leading to reduced vision in one eye. Strabismus, on the other hand, refers to misalignment of the eyes, disrupting binocular vision. While Amblyopia is often a consequence of untreated Strabismus, they can exist independently. Strabismus presents as an ocular misalignment, whether esotropia (inward deviation), exotropia (outward deviation), or hypertropia (upward or downward deviation).
Amblyopia and Strabismus are caused by a complex interaction of genetic predisposition and environmental circumstances. Amblyopia is often caused by childhood problems that cause blurred or uneven vision, such as refractive defects or eye misalignment. Strabismus, a common cause of amblyopia, affects binocular vision and impairs depth perception. If left untreated, these disorders can have long-term effects on visual function, compromising academic performance, occupational opportunities, and general quality of life.
Corrective lenses, tailored to address refractive errors or misalignment, offer an initial line of defense. Eye patches, strategically employed to occlude the stronger eye, stimulate visual development in the weaker eye, a cornerstone in Amblyopia management. Surgical interventions, precise and nuanced, rectify ocular misalignment in Strabismus, restoring binocular function and averting further visual degradation.
Vision therapy, a systematic and individualized approach, engages patients in exercises designed to enhance eye coordination, visual perception, and overall ocular function. Eye exercises, encompassing convergence exercises and activities to improve eye movement control, augment the efficacy of clinical interventions, fostering a harmonious fusion of clinical precision and holistic empowerment.
Cataracts appear as a common yet formidable opponent within the complicated lens of ocular pathology. Cataracts, which are caused by the gradual clouding of the eye's natural lens, obstruct light transmission, resulting in impaired or poor vision. Cataracts are caused by a complex combination of age-related changes, genetic predisposition, and environmental variables. Smoking, heavy alcohol intake, and prolonged exposure to ultraviolet (UV) radiation all increase the risk, emphasizing the importance of doing a thorough risk assessment.
The modest signs of cataracts, which are frequently concealed in the early stages, crystallize into recognizable symptoms as the condition worsens. Cataracts have a significant impact on daily visual experiences, ranging from gradual blurring to increased sensitivity to light. Colors may lose their brilliance and night vision may be impaired. If left untreated, the cumulative effect can become a severe obstacle to normal tasks, underlining the importance of careful detection and quick intervention.
The gold standard for proven clinical solutions is cataract surgery, which provides a revolutionary approach to restoring visual acuity. The clouded lens is removed during this precise surgical process, and an artificial intraocular lens (IOL) is inserted to replace it. Individual visual needs are taken into account while selecting an IOL, which can range from monofocal to multifocal. This allows for a personalized approach to postoperative vision. This surgical procedure, which is frequently performed as an outpatient, has a remarkable success rate.
Holistic techniques weave into the story of cataract care as a complement to professional precision. Antioxidant-rich diets high in vitamins C and E, as well as lutein and zeaxanthin, provide a protective shield against oxidative stress, potentially lowering the likelihood of cataract formation. The inclusion of UV protection measures into daily life, stressing the usage of sunglasses and caps to prevent exposure to damaging ultraviolet rays, is also critical. This combination of clinical knowledge and proactive lifestyle choices emphasizes the holistic approach to cataract treatment.
The convergence of holistic and clinical practices offers a dynamic tapestry for comprehensive care. Understanding the commonalities and distinctions between these approaches is pivotal for cultivating a nuanced strategy tailored to individual needs.
Holistic and clinical approaches share a fundamental commitment to enhancing and preserving eye health. Holistic practices, including lifestyle modifications, nutrition, and stress management, recognize the interconnectedness of overall well-being and ocular vitality. Clinical interventions, such as surgeries and medications, target specific eye conditions with precision. While both approaches converge on the overarching goal of optimizing vision, they differ in scope and methodology. Holistic practices cast a wide net, addressing broader health factors that influence eye health, while clinical interventions provide targeted solutions for diagnosed ocular conditions. It's the synthesis of these approaches that ensures a well-rounded strategy for sustained eye health.
Navigating the complexity of eye health requires a multidisciplinary approach. We urge interdisciplinary approaches combining optometrists, ophthalmologists, dietitians, and stress management specialists. The eyes are not independent entities; they are vital to your overall health. A thorough understanding is required, taking into account elements such as systemic health, nutrition, and stress levels. We build a strong framework that goes beyond the immediate emphasis on ocular diseases by encouraging collaboration among diverse healthcare specialists. This multidisciplinary collaboration guarantees that your eye health is treated holistically, recognizing the delicate connection between several aspects of your health.
The Anywhere Healing Alpha Heal Device heralds a new era in ocular care, epitomizing the intersection of cutting-edge technology and therapeutic innovation. This compact yet powerful device is designed to seamlessly integrate into the daily lives of individuals seeking to enhance and preserve their vision. It represents a paradigm shift, transcending the conventional boundaries of eye health management by placing the reins of control firmly in the hands of the individual.
At the core of the Anywhere Healing Alpha Heal Device is its capacity to deliver targeted and non-invasive healing frequencies directly to the eyes. This innovative technology operates on the premise of stimulating cellular regeneration and optimizing the function of ocular tissues. By harnessing the power of bioresonance, the device aims to address a spectrum of ocular conditions, from refractive errors to degenerative diseases. Its potential benefits extend beyond mere symptom alleviation, fostering a proactive and holistic approach to eye health by promoting cellular vitality and resilience.
The efficacy of the Anywhere Healing Alpha Heal Device is supported by convincing case studies and testimonials. Individuals who have adopted this device into their eye care routine report significant gains in visual acuity, decreased reliance on external assistance, and an improved overall sense of ocular well-being.
These testimonies highlight the device's adaptability, appealing to a wide spectrum of people with varied eye health concerns. The Anywhere Healing Alpha Heal Device emerges as a light of hope and empowerment in the area of eye health, from the treatment of refractive defects to the assistance of more complex illnesses. The Anywhere Healing Alpha Heal Device is a tribute to the relentless quest of innovation in the changing field of emerging technology.